Information Sheet for Colonoscopy Patients
ENDOSCOPY
5/7/20244 min read
Colonoscopy: Nothing to be Scared about
Thank you for booking your colonoscopy. I appreciate your trust in me as your colonoscopist and promise to do all that I can to make sure you have an accurate, effective and comfortable examination. The purpose of this brochure is to explain a few things to you before the day of the examination, so that you arrive with a good understanding of what will be taking place.
1. The colon
The colon (the large intestine) is a six foot long muscular tube that runs around the outer edges of the abdominal cavity. Because most people’s abdomens are small it needs to be coiled to fit. This creates bends and loops that can be made worse during insertion of the colonoscope.
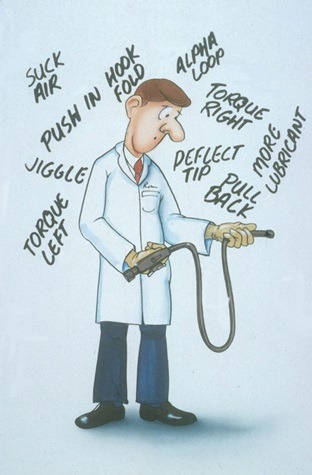
The colon doesn’t mind having a scope inserted; that is not painful. Stretching the colon is painful, and stretching occurs when the natural looping is exaggerated by pushing the scope in. My technique of colonoscope insertion concentrates on shortening the colon over the scope just like you would bunch up a stocking before you pull it over your foot. The more I can do this the less pain you will have.
Everybody’s colon is different: different lengths, different loopyness, different floppiness, different fixedness from adhesions, and different sensitivity. In general ladies have longer and floppier colons than men. A person’s first colonoscopy is the time when they find out how “colonoscopy friendly” their colon is. Some patients have no pain at all, while others (a small minority) have a lot of pain.
2. Sedation
There are two ways to do colonoscopy:
i. Just find the longest scope you can and push it in til you reach the end. This is easy to learn but makes big loops, is painful and dangerous. Patients must be knocked out.
ii. Try to minimize loops and minimize air, by turning the patient and applying abdominal pressure to stop looping. This is hard to learn, but needs less sedation and produces a safer and more accurate examination. This is my technique.
So for first time patients, I prefer to use a modest initial dose of sedative and see what the colon is like. I add sedation and narcotics as necessary. For the patient’s next examination I already know if the first exam was easy or hard, pain-free or painful, so I can begin with a more appropriately tailored dose of medication. Some patients have such friendly colons that they don’t need any sedation. This allows them to return to work immediately after the procedure, and to drive themselves to and from the appointment.
3. Bowel Prep
Having a clean colon is a key to a comfortable, accurate colonoscopy. If there are chunks of stool, the exam takes longer, more air is needed so the colon is lengthened and loops are exaggerated so the exam is more painful, and polyps may be hidden by the stool. In addition if a big polyp is found it may be dangerous to remove it. This is because if there is a perforation in a “dirty” colon stool gets out of the colon into the abdomen.
There are two reasons for a dirty colon:
1. Not all the stool was cleaned out
2. The colon was clean but then became dirty again as bile came down from the small bowel
To avoid 1., take your prep as instructed. All preps are effective if taken as instructed. If you have chronic constipation and are on regular laxatives, take an extra dose the day before the bowel prep to make sure that the colon is not loaded. If you have diverticulosis (the pockets), you may have stool balls in your colon after the prep is done. This is not your fault. The stool hides in the pockets while the prep is working and then comes out afterwards. If this has been a problem in the past take a dose of senokot before starting the prep.
To avoid 2., take your prep within 3 or 4 hours of the examination. If you have an appointment before 11.00am, take all the prep the night before. For an appointment from 11.00am to 1.pm, take half the prep the night before and half the morning of the exam (split prep). For an exam after 1.00 pm, take all the prep the morning of the exam. I also prescribe 2 Imodium tablets to be taken at the end of the diarrhea caused by the prep. This will stop bile coming out of the small intestine and ruining your good work.
The Procedure:
After insertion of an IV, baseline vital signs and informed consent are obtained, and you are placed on your back with your knees bent. Sedation is given and some lubricating jelly is placed around your bottom. The scope is gently inserted. As gas enters the rectum you may feel an urge to pass it out. This is fine; go ahead. As the scope goes through the sigmoid (the bendiest part of the colon) you may feel cramps. These usually pass in a few seconds. You will also feel the presence of the scope in the anus; not painful but just “intrusive”. The scope then passes up the left side of the colon, across the top of the abdomen (transverse colon) and down the right side to the cecum. This is the end of the road. Along the way there are corners. Passing the scope around a corner may involve you holding your breath, having a nurse push on your tummy, or you turning from one side to the other. All these techniques are designed to minimize pain and the need for sedation. Having reached the cecum the scope is pulled out and a thorough inspection takes place. Polyps are removed as they are seen; small ones with forceps and larger ones with a snare. The whole examination averages 22 minutes. Afterwards you will spend time in recovery and I will discuss what we found and when your next examination should be.
Thank you again for trusting me with your colon. I shall treat it as if it were my own.
James Church